Surgical Treatment of Type 2 Diabetes
Advanced metabolic procedures can enhance insulin secretion and sensitivity, improving glycaemic control in obese and non‑obese patients and helping prevent long‑term complications.
Metabolic Focus
GLP‑1 mediated, physiologic
Minimally Invasive
Laparoscopic approach
Rapid Effects
Often within days
Why consider surgery?
- Difficult glycaemic control despite diet, exercise and medications
- Risk of microvascular complications: retinopathy, nephropathy, neuropathy
- Potential for medication reduction after procedure (individualised)
Type 2 Diabetes is a Growing Epidemic
Type 2 Diabetes (DM 2) is increasing worldwide and associated with serious complications including vision loss—blindness rates are reported far higher in diabetes than in the general population. Intensive management yields more years free of microvascular and neurologic complications and improves overall life expectancy.
Around 80% of people with DM 2 are overweight or obese; weight reduction helps control, but conventional therapy may not normalise sugars in many patients.
Care in Mumbai
Metabolic procedures are now performed in Mumbai by Dr Abhay Agrawal and team. Typical operating time is ~4 hours; walking usually begins the next day with return to work often in about a week (as advised individually).
How Metabolic Surgery Works
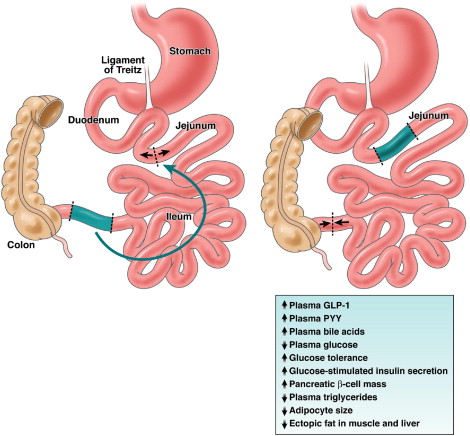
Research highlights the role of intestinal hormones—especially GLP‑1—on pancreatic β‑cells and insulin secretion in response to food. A technique popularised by Dr Aureo de Paula repositions a segment of ileum to the upper small intestine (ileal interposition). When food reaches this segment sooner, GLP‑1 is released rapidly, boosting insulin in a physiologic, meal‑dependent manner (so hypoglycaemia risk is minimised in the fasting state).
- Effects often occur within days—before significant weight loss
- In moderately obese patients, sleeve gastrectomy (LSG) may be combined to aid weight control
- In normal‑BMI patients, ileal interposition aims to improve diabetes without undesired weight loss
Physiologic Benefits
- Post‑prandial insulin surge improves glucose control
- Improved insulin sensitivity may reduce fasting glucose
- No intestinal length loss; food passage remains physiologic
- No routine long‑term malabsorption expected
Who May Benefit
- Type 2 diabetes with inadequate control on diet/medications or insulin
- Normal BMI (ileal interposition without excessive weight loss)
- BMI 22–34 in studies; selection is individualised
- C‑peptide typically > 1 (reflects insulin reserve)
- HbA1c often > 8 suggests poor control pre‑op
Our care team evaluates risks, expected benefits and suitability based on labs, imaging and medical history.
Potential Improvements
- Reduced/ceased diabetes medications (case‑dependent)
- Better lipids (triglycerides, cholesterol)
- Improved kidney function markers (where applicable)
- Relief of neuropathic leg pains
Evidence & Outcomes
Reports from Brazil and international presentations describe high remission rates after ileal interposition, including series by Dr Aureo de Paula (700+ cases over ~7 years, 95% remissions as presented; publications include Surgical Endoscopy). Multiple Brazilian centres (≈ 2000 patients total) have contributed experience in this technique.
A study in non‑morbidly obese patients (BMI ≈ 22–34; mean 26.6) with long‑standing, poorly controlled DM 2 reported ~92.9% achieving adequate glycaemic control at ~9.2 months mean follow‑up, with no reported complications in that cohort.
Note: Outcomes vary; remission definitions and follow‑up durations differ among studies. Your surgeon will discuss evidence and what it means for you.
Quality of Life
- Potential earlier return to daily activity (typically walk next day)
- Many return to work in ~1 week (as advised)
- Focus on preventing long‑term diabetic complications
Procedural Options
Ileal Interposition
Gold‑standard weight‑loss & metabolic results.
Ileal Interposition + LSG
Adds sleeve gastrectomy for moderate obesity to aid weight control alongside metabolic benefits.
Individualised Variants
Technique tailored to BMI, C‑peptide, HbA1c, comorbidities and goals after multidisciplinary review.
Risks, Safety & Hospital Course
All surgery carries risk (bleeding, infection, anastomotic issues, DVT/PE, anaesthesia‑related events). Laparoscopic methods aim to reduce pain and hospital stay. Expect ~5 days of observation post‑op to monitor falling sugars and adjust medications.
Costs reflect advanced staplers, energy devices and experienced team. Your surgeon will detail risks, alternatives and expected recovery for your situation.
Not Medical Advice
This page is informational and not a substitute for personalised medical advice. Decisions should be made after consultation and appropriate tests.
Long‑Term Complications of DM 2
Cardio‑cerebral
Higher risk of heart disease and strokes over time.
Renal
Progression to kidney disease/failure may require dialysis or transplant.
Neuropathy
Nerve damage can affect digestion, bladder, sexual function and limbs.
Foot Health
Ulcers and poor circulation can lead to amputations.
Vision
Retinopathy, glaucoma and cataracts increase blindness risk.
Metabolic Syndrome
Often coexists with hypertension, dyslipidaemia, fatty liver and PCOS.

About Dr. Abhay Agrawal
Dr. Agrawal is a Laparoscopic GI & Bariatric Surgeon in Mumbai offering comprehensive, personalised care from consultation through recovery. His approach blends advanced technique with a compassionate bedside manner.
- Expertise
- Comprehensive Support
- Personalised Care
Over 25 years of experience and hundreds of successful surgeries with state‑of‑the‑art technology and transparent communication.
Real Patient Stories
Frequently Asked Questions
Is metabolic surgery suitable if I’m not obese?
Yes, selected normal‑BMI patients with Type 2 Diabetes and adequate insulin reserve (e.g., C‑peptide > 1) may be considered for ileal interposition, aiming to avoid undesired weight loss.
Will I still need diabetes medications?
Many patients reduce or stop medications within weeks to months; this is individual and guided by your care team with close glucose monitoring.
How long is the hospital stay?
Typically around five days for observation and therapy adjustment, though this varies by patient and clinical progress.
Is there malabsorption or nutritional deficiency?
Ileal interposition is designed without intestinal shortening or diversion, so long‑term malabsorption is not expected. Nutritional follow‑up still matters.
What changes after surgery?
Portion sizes are smaller per meal; follow prescribed diet progression and activity plan. Regular follow‑up supports durable results.
